|
|
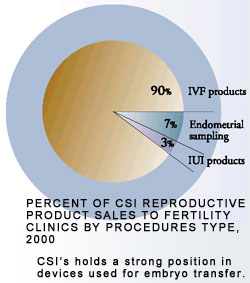 Products used to treat reproductive disorders in fertility clinics represent 11 percent of CSI revenue, primarily for fertility assessment and treatment. Infertility is defined as the failure of a couple to establish a pregnancy after one year of unprotected intercourse. This is based on expected monthly conception rates of 20-25 percent in healthy young couples [12] . Fertility decreases significantly in women over the age of 35 [13] . Approximately 15 percent of couples are infertile and in 15 percent of these cases, no cause can be identified [14]. Increased infertility in the U.S over the past 25 years is due to an increase in sexually transmitted diseases and the deferral of childbearing to later years. In addition, increased public information regarding new treatments and a greater willingness to discuss fertility issues openly have caused more couples to seek treatment. Basic infertility evaluations can identify the cause in approximately 85 percent of couples. [15] Fertility Procedures
Cervical and coital factors: Abnormalities
in cervical mucus combined with other causes can contribute to infertility.
For example, disruption or removal of cervical epithelium during surgical
procedures may narrow the cervical opening or cause inadequate mucus production,
compromising the mechanism for sperm transport and storage.
Clinicians use postcoital testing to assess cervical and coital factors. This test, usually performed early in the assessment, evaluates mucus quality and sperm-mucus interaction through visual and microscopic observations. The CSI Aspirette endocervical suction curette helps physicians collect clean samples. Additional early infertility testing includes a Pap smear and cervical cultures to evaluate potential underlying sexually transmitted infection. 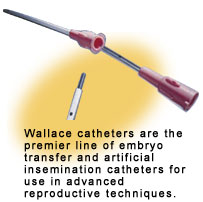 Intrauterine
insemination using an injection catheter has achieved high pregnancy rates
in couples with cervical factor infertility caused by structural abnormalities.
CSI offers two artificial insemination catheters, the Uni-Sem and
the Wallace. The nature of the condition and the preference of the
physician determine which is used. Intrauterine
insemination using an injection catheter has achieved high pregnancy rates
in couples with cervical factor infertility caused by structural abnormalities.
CSI offers two artificial insemination catheters, the Uni-Sem and
the Wallace. The nature of the condition and the preference of the
physician determine which is used. 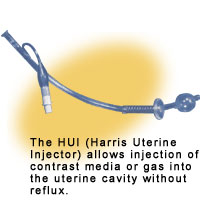 Uterine Factors: Reduced fertility has
been associated with many uterine conditions including chronic endometritis,
benign tumors, adhesions, congenital malformations and polyps. Endometritis,
an inflammation of the endometrial lining, interferes with ovum implantation.
The other conditions prevent either implantation or the proper endometrial
development that is essential in providing nutrients for sustained growth.
Endometritis is identified by endometrial biopsy and culture. Uterine Factors: Reduced fertility has
been associated with many uterine conditions including chronic endometritis,
benign tumors, adhesions, congenital malformations and polyps. Endometritis,
an inflammation of the endometrial lining, interferes with ovum implantation.
The other conditions prevent either implantation or the proper endometrial
development that is essential in providing nutrients for sustained growth.
Endometritis is identified by endometrial biopsy and culture. X-ray of the uterus and fallopian tubes after injection of a contrast dye identifies other causes. The dye is injected using a specially designed catheter fitted with a balloon to prevent leakage from the cervical canal. CSI offers several disposable dye injection catheters to accommodate variations in cervical and uterine size including the HUI, HUI MiniFlex and ZUI uterine injectors. CSI also provides a disposable procedure kit that contains the items essential for catheter introduction. 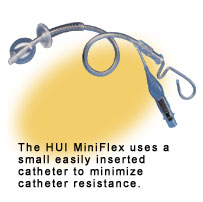 Fallopian
tube factors: Tubal infertility results when the ovum cannot descend
into the uterine cavity. It is evaluated using either an X-ray procedure
or through laparoscopic surgery. One of the most common causes of infertility
is distal (the section closest to the ovary) fallopian tube disease. Treatment
includes operative laparoscopy or, in extreme cases, an open procedure.
Successful pregnancies occur in 5-30 percent for moderate to severe disease
and 50-70 percent in mild cases [16]. There are fewer
patients with proximal (nearest the point of attachment) tubal disease.
Several surgical procedures are used for proximal tube repair and successful
pregnancies have occurred in 20-40 percent of these patients [17]. Fallopian
tube factors: Tubal infertility results when the ovum cannot descend
into the uterine cavity. It is evaluated using either an X-ray procedure
or through laparoscopic surgery. One of the most common causes of infertility
is distal (the section closest to the ovary) fallopian tube disease. Treatment
includes operative laparoscopy or, in extreme cases, an open procedure.
Successful pregnancies occur in 5-30 percent for moderate to severe disease
and 50-70 percent in mild cases [16]. There are fewer
patients with proximal (nearest the point of attachment) tubal disease.
Several surgical procedures are used for proximal tube repair and successful
pregnancies have occurred in 20-40 percent of these patients [17].
Many patients with severe disease or with a history of previously unsuccessful tubal surgery consider in vitro fertilization (IVF) as an alternative. IVF, the most frequently used assisted reproductive technology (ART), involves manipulation of eggs and embryos outside of the body. Fertilized eggs are then returned into the body to establish pregnancy. These complex procedures are performed in fertility clinics, as they require a highly specialized team of clinicians. In IVF, a hormone mixture stimulates the ovaries to maximize the production of oocytes (eggs not yet completely developed). An oocyte retrieval needle collects the eggs under ultrasonic guidance. They are placed with sperm in media conducive to fertilization. Two or three days later, the embryos are graded. Those chosen for transfer are introduced into the uterus with a special transfer catheter. CSI's Wallace product line leads the United States embryo transfer catheter market. Other Wallace products include insertion stylets, trial transfer catheters and the recently introduced oocyte retrieval needle. Peritoneal factors: Peritoneal related infertility factors (those related to the lining of the abdominal cavity) include pelvic inflammatory disease, endometriosis, ruptured appendix, ruptured ovarian cyst, previous surgery, and foreign body reaction. Adhesions (a fibrous band holding together parts that are usually separated) resulting from these processes can involve the fallopian tubes or ovaries and interfere with normal oocyte delivery. To minimize further adhesion formation, diagnostic evaluation and treatment is usually performed laparoscopically. Endometriosis is the presence of endometrial tissue outside of the uterine cavity. Although benign, it can invade and destroy tissue causing severe inflammation and adhesions. About 7 percent [18] of women of reproductive age in the United States have some form of endometriosis. About 30 percent [19] of infertile women who are otherwise normal have this condition. Endometriosis is either monitored with "watchful waiting" or treated using hormonal therapy or surgery, depending on the patient's age, desire for childbearing, severity of symptoms and coexisting medical conditions. Conservative surgical procedures include excision, vaporization and coagulation of endometrial implants and removal of adhesions using laparoscopy.
Basic Infertility Evaluations
Ovulatory factors: Patients with ovulatory
disorders complain of amenorrhea (lack of menses), menorrhagia (abnormal
bleeding) or infertility. Diagnosis is through hormone level testing, basal
body temperature measurement, endometrial biopsy and early fertility evaluation.
Treatment includes ovulation induction with agents such as clomiphene citrate.
Follicle development is often monitored using ultrasound. Endometrial biopsies
are also recommended, as up to 25 percent [20]of menstrual
cycles induced by clomiphene citrate produce an endometrial environment
unfriendly to implantation. In addition, cervical mucus is evaluated during
therapy, as approximately 15 percent [21] of patients
develop dysfunctional mucus production requiring intrauterine insemination.
The pregnancy rate for this therapy is only about 40 percent [22],
so ovulatory induction is frequently used in conjunction with intrauterine
insemination.
Male factors: Male infertility causes nearly half of all couples' inability to conceive. Several mechanisms may cause this, including abnormal sperm production, disordered sperm maturation, abnormal sperm function or ineffective sperm delivery. Unfortunately, medical or surgical treatment is appropriate in only 10 percent of these cases and assisted reproductive technologies offer the best opportunity for conception. CSI does not currently offer any specific products for evaluation of male infertility. 12Moghissi KS, ed. Infertility. In: Holzman, GB, ed. Precis, Reproductive Endocrinology: An Update in Obstetrics and Gynecology. Washington, ACOG, 1998; 71. 13Ibid; 71. 14Ibid; 71. 15Ibid; 71. 16Infertility. In Visscher HC, ed. Precis V, An Update in Obstetrics and Gynecology. American College of Obstetrics and Gynecology, 1994; 424. 17Ibid; 425. 18Moghissi KS, ed. Infertility. In Holzman GB, ed. Precis, Reproductive Endocrinology: An Update in Obstetrics and Gynecology. Washington, ACOG, 1998; 79. 19Ibid; 80. 20Ibid; 84. 21Ibid; 84. 22Ibid; 84. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
||||||